Research Corner
- Detecting Unique Spectral Fingerprints in Cough Sounds for Diagnosing Respiratory Diseases
- Can Cough Hypersensitivity Symptom Profiles Distinguish Chronic Cough Phenotypes?
- Assessing the impact of acid-suppressive medications on non-specific chronic cough
- Bias-free AI model for respiratory disease diagnosis using cough audio
- The Interplay of asthma and chronic cough
- Chronic Cough: Updated Guidelines, Innovative Approaches, and Emerging Treatments
- Debates Surrounding Antibiotic Treatment for Chronic Wet Cough in Pediatric Patients
- Somatic points for cough and urge to cough in chronic coughers
- An Aero digestive approach to chronic cough in children
- Structural and functional changes in the higher cortical regions brain due to chronic refractory cough
- Effect of adenoidectomy on cough reflex sensitivity in children
- The patients’ perspective of chronic refractory cough
- Considering the multi-disciplinary approach in the management of chronic cough in children
- Assessment of the efficacy of pulmonary function test for accurate diagnosis of pediatric asthma and cough variant asthma
- Pediatric chronic productive cough: Are antibiotics the solution?
- Cough sensitivity: Evaluation methods and influencing factors
Detecting Unique Spectral Fingerprints in Cough Sounds for Diagnosing Respiratory Diseases
Introduction:
Coughing is a common symptom associated with various illnesses, including COVID-19. Researchers are investigating the potential of using cough sound signals for a cost-effective method of disease diagnosis. Unlike traditional diagnostic methods, which are often expensive and require specialized personnel, smartphone-based cough analysis offers a more accessible alternative.
Objective:
To examine the feasibility of using acoustic analysis of cough sounds for diagnosing respiratory ailments, including COVID-19, pneumonia, and asthma.
Methods:
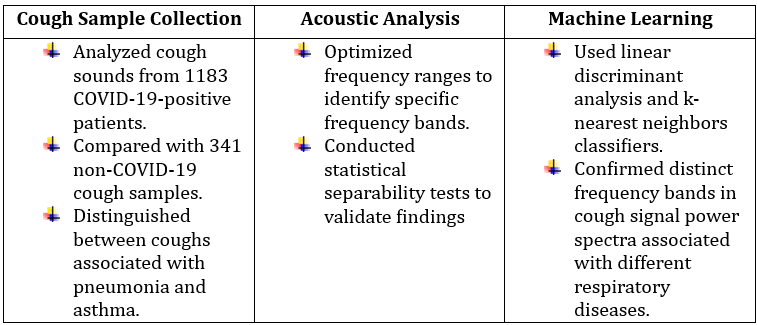
Results:
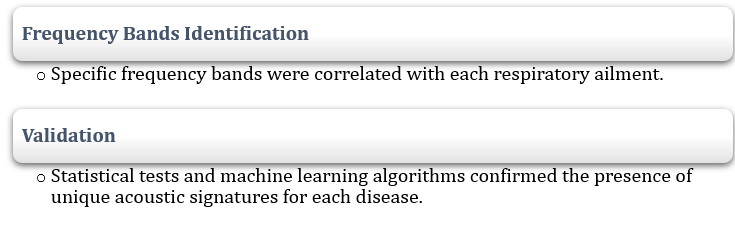
Conclusion:
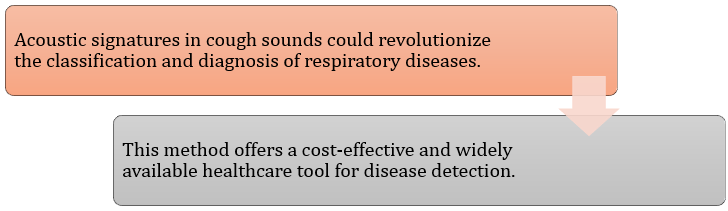
To know more: https://doi.org/10.1038/s41598-023-50371-2
Reference: Ghrabli S, et al. Identifying unique spectral fingerprints in cough sounds for diagnosing respiratory ailments. Scientific Reports. 2024 Jan 5;14(1):593.
Can Cough Hypersensitivity Symptom Profiles Distinguish Chronic Cough Phenotypes?

A recent study has explored whether cough hypersensitivity symptoms can distinguish between different phenotypes of chronic cough. The research focused on asthmatic chronic cough and refractory chronic cough (RCC), assessing symptom triggers and throat sensations in patients with these conditions.
Key Findings:
- Cough reflex hypersensitivity has been proposed as a common feature of chronic cough in adults, but its clinical characteristics across different chronic cough phenotypes remain unclear.
- The study analyzed data from 280 patients over six months from the Korean Chronic Cough Registry.
- 79 patients had asthmatic cough (cough variant asthma or eosinophilic bronchitis).
- 201 patients had refractory chronic cough (RCC).
- Symptom assessment was performed using the Cough Hypersensitivity Questionnaire (CHQ) and the Leicester Cough Questionnaire (LCQ) to measure cough-specific quality of life.
Results:
- CHQ scores were similar between the two groups:
- Asthmatic cough: 8.3±3.7
- RCC: 8.9±3.9
- No significant difference was observed (p=0.215).
- There were no significant differences in LCQ and cough severity VAS scores between the groups.
- Both groups showed a negative correlation between cough hypersensitivity and quality of life:
- Asthmatic cough: r = -0.427, p<0.001
- RCC: r = -0.306, p<0.001
Conclusion:
The study suggests that cough hypersensitivity symptoms may not distinguish between asthmatic chronic cough and RCC, pointing to a shared mechanism in cough pathogenesis across these phenotypes, despite potentially different treatable traits. Chronic cough appears to be the primary diagnosis for both conditions.
Cough Hypersensitivity Symptoms May Not Differentiate Between Asthmatic and Refractory Chronic Cough
To know more: https://doi.org/10.1183/23120541.00260-2024
Reference: Kim MY, et al. Could cough hypersensitivity symptom profile differentiate phenotypes of chronic cough. ERJ Open Research. 2024 Jan 1.
Assessing the impact of acid-suppressive medications on non-specific chronic cough

Non-specific chronic cough, a persistent cough without a clear cause, affects approximately 9.6% of the global population and significantly impacts quality of life. Recognized by the Montreal consensus as an extra-esophageal manifestation of gastroesophageal reflux disease (GERD), it is also linked to asthma and post-nasal drip. Despite these associations, the efficacy of proton pump inhibitors (PPIs) for treating chronic cough remains controversial. A 2011 meta-analysis found insufficient evidence supporting PPIs for this condition.
Recent research, based on nine placebo-controlled randomized trials, found that PPIs slightly reduced cough severity. However, sensitivity analysis indicated that excluding a major study with a large sample size affected the statistical significance of the results. The study also showed similar effects of PPIs on cough severity in patients with both non-specific chronic cough and laryngopharyngeal reflux, with no significant reduction observed due to small sample sizes and wide confidence intervals. Improvement was more pronounced in patients with abnormal reflux on pH monitoring. Extended treatment durations did not enhance outcomes, and quality of life improvements were modest and not statistically significant. Mechanistic theories suggest that PPIs may not fully alleviate symptoms due to non-acidic reflux, and long-term PPI use has been linked to potential risks, including increased community-acquired pneumonia.
To Know More: https://doi.org/10.1038/s41598-024-62640-9
Reference: Floria DE, et al. Systematic review and meta-analysis: proton pump inhibitors slightly decrease the severity of chronic cough. Scientific Reports. 2024 May 25;14(1):11956.
Bias-free AI model for respiratory disease diagnosis using cough audio

A new AI-based diagnostic tool, called the Bias-Free Network (RBF-Net), offers a solution to a major challenge in cough-based diagnosis of respiratory diseases (RDs). Many existing models overlook confounding variables, such as age, gender, and smoking status, which can lead to biased predictions and unreliable performance. To tackle this issue, RBF-Net uses a hybrid of Convolutional Neural Networks (CNN) and Long Short-Term Memory (LSTM) networks, along with a bias predictor that employs a conditional Generative Adversarial Network (c-GAN). This setup helps mitigate the impact of confounders in the training data, ensuring more accurate RD diagnosis.
Incorporating COVID-19 data, RBF-Net was tested on unbalanced datasets with confounding factors, including gender, age, and smoking status. It achieved test set accuracies of 84.1%, 84.6%, and 80.5%, respectively, outperforming a traditional CNN-LSTM model by 5.5%, 7.7%, and 8.2%.
The results highlight RBF-Net’s robustness in biased training conditions, offering a significant improvement in reliability for AI-driven respiratory disease diagnostics.
This advancement holds promise for more accurate, unbiased predictions, providing valuable support for healthcare professionals.
To Know More: https://doi.org/10.3390/bioengineering11010055
Reference: Saeed T, et al. An AI-enabled bias-free respiratory disease diagnosis model using cough audio. Bioengineering. 2024 Jan 5;11(1):55.
The Interplay of asthma and chronic cough

To know more: Martins P, et al. Asthma and chronic cough: two related conditions. Journal of Allergy and Clinical Immunology. 2024 Feb 1;153(2): AB23.
Chronic Cough: Updated Guidelines, Innovative Approaches, and Emerging Treatments
At the end of 2023, updated national clinical statements on chronic cough were released by both Australia and the UK, marking significant updates after 13 and 17 years, respectively. Chronic cough, defined as lasting 8 weeks or more, is common, especially among middle-aged women, and severely impacts quality of life.
The initial assessment of chronic cough should include clinical history, examination, and a chest X-ray to rule out acute infections, ACE inhibitor usage, and classical conditions such as asthma and gastroesophageal reflux disease (GERD). Further investigations may involve spirometry, a full blood count, fractional exhaled nitric oxide, and possibly a computed tomography scan based on red flags and risks for serious conditions.
Traditional management models, which focus primarily on asthma, GERD, and rhinosinusitis, are increasingly seen as inadequate. A new paradigm suggests that chronic cough may be a neuroinflammatory or neuropathic disorder, with cough hypersensitivity as a central issue. This model is supported by evidence such as increased airway sensory nerve fibers, patient-reported triggers, functional MRI findings, and similarities to CANVAS syndrome.
Recent advancements in treatment include repurposed medications like morphine, gabapentin, and pregabalin, as well as novel agents like P2X3 inhibitors (e.g., Gefapixant). Non-pharmacological approaches, such as behavioral techniques from speech therapists and respiratory physiotherapists, have also shown promise.
The clinical approach should focus on excluding serious causes to reassure patients, tailoring investigations to the clinical context, and avoiding empirical treatments without specific indications. Treatment should target identified treatable traits and the underlying issue of cough hypersensitivity.
The updated guidelines aim to improve systematic approaches, recognize chronic cough as a distinct disease, and enhance patient outcomes.
To know more
https://doi.org/10.1111/resp.14686
Debates Surrounding Antibiotic Treatment for Chronic Wet Cough in Pediatric Patients

https://doi.org/10.1016/j.jpeds.2023.113762
Somatic points for cough and urge to cough in chronic coughers

Recently, a group of researchers documented a case of a patient with chronic cough who reported an urge to cough (UTC) or coughing triggered by light pressure on the sternocleidomastoid muscle and sternum, and on the lower cervical or first dorsal vertebrae, as well as by pressure on the jugular notch and neck movements.
Based on this, the researchers conducted a clinical investigation of this coughing pattern in both chronic coughers and controls.
Methods
- The study included 58 adult outpatients with consecutive chronic cough and 34 healthy controls.
- The researchers attempted to trigger coughing and/or the UTC feeling by applying finger pressure to specific spots on the chest and neck, as well as by having the patient move their neck fully up and down.
- An area on the upper trunk or neck that caused a UTC feeling or visible coughing in response to mechanical stimulation was referred to as a “somatic point for cough” (SPC).
- Participants with at least one SPC were considered SPC+ while those with no identifiable SPC were classified as SPC-.
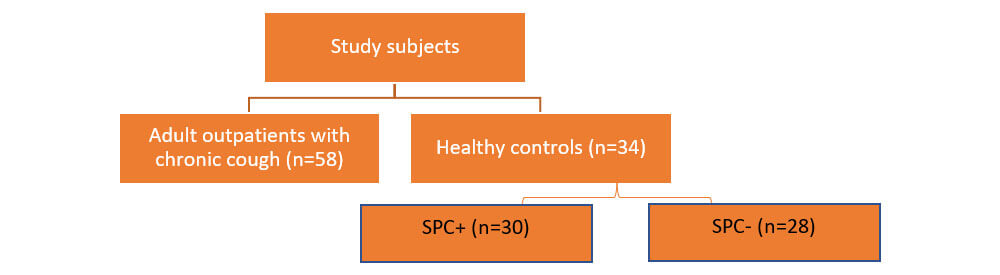
- A calibrated force sensing resistor (Ohmite FSR03, Warrenville, IL) attached to the tip of the investigator’s first finger was used to measure the minimum pressure required to trigger UTC or coughing.
- Patients rated the intensity of the UTC experienced by means of a visual 0–9 scale (VAS).
Results
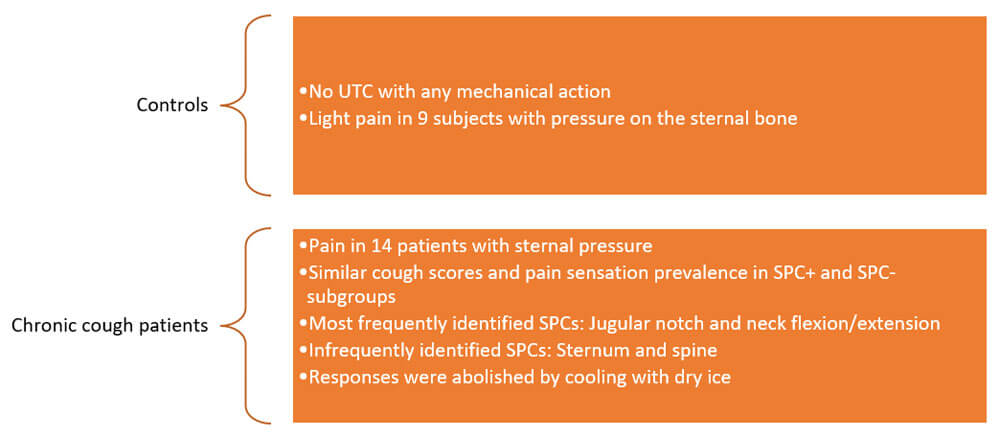
The significant proportion of patients with chronic cough who also present with SPC suggests that this symptom plays a significant role in the development and continuation of the condition. The reason why only specific mechanical stimulation of somatic areas can trigger UTC or cough remains unknown.
Reference:
Mannini C, Bernacchi G, Bonti V, et al. Somatic points for cough and urge to cough in chronic coughers. Respir Med. 2022;200:106929.
An Aero digestive approach to chronic cough in children

- A pediatric chronic cough is defined as a persistent cough lasting for over 4 weeks in children aged <14 years.
- Chronic cough can be classified into different categories based on its diagnosis, management techniques, or presenting symptoms.
- A common paradigm is to classify cough as normal (expected), specific (with cough pointers), and nonspecific types.
- A group of researchers focused on the diagnostic process for children with chronic cough in outpatient settings, as the challenge in pediatric cough diagnosis lies in its varied causes and frequent coinciding symptoms.
Cough evaluation by the aerodigestive team
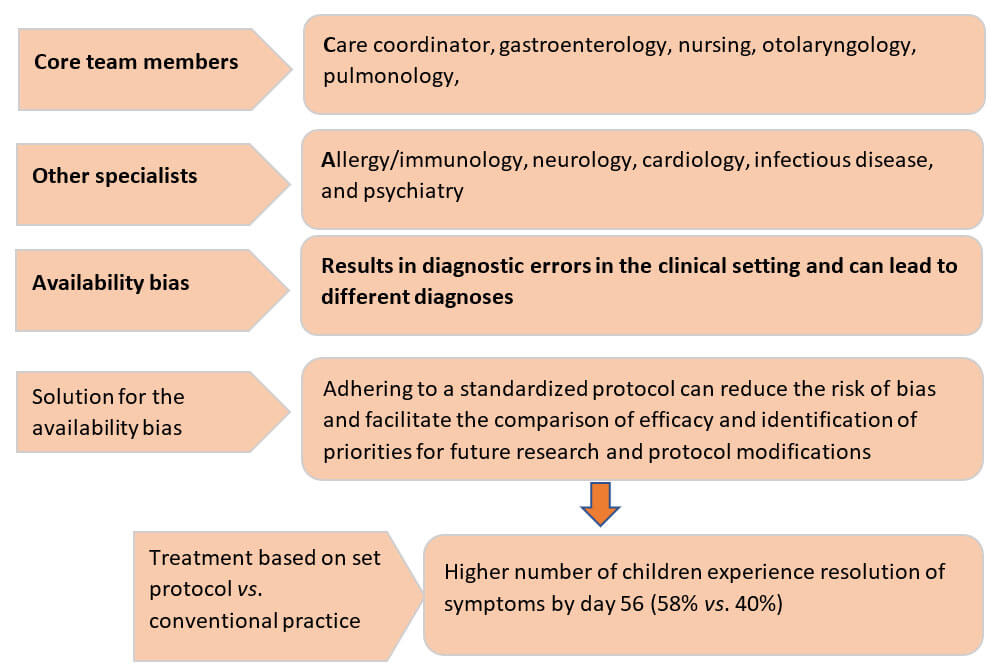
Key questions to ask when diagnosing and treating pediatric chronic cough
1. Does the cough have specific pointers, classic features, or chest radiograph and spirometry abnormalities?
If so, then consider treatments for diseases associated with specific pointers, if not, then continue as following:
a. Classic coughs include the croupy/barking cough of tracheomalacia, the staccato cough for chlamydia, cough with casts, and the whoop for pertussis.
b. Assess risk factors for foreign body inhalation and contributions from rhinosinusitis and reflux.
2. Is the cough wet?
If so, consider treatment of protracted bacterial bronchitis.
a. Consider checking immune status, pertussis, and mycoplasma.
3. Is the cough dry?
If so, consider inhaled corticosteroids for 2 weeks for asthma/ asthma-like illnesses.
A comprehensive evaluation by an aerodigestive team leads to improved care and reduces the risk of specialty availability bias.
Reference:
Jiang ZY, Gatcliffe C, Mai T, et al. Aerodigestive approach to pediatric chronic cough. Otolaryngol Clin North Am. 2022;55(6):1233–1242.
Structural and functional changes in the higher cortical regions brain due to chronic refractory cough

Chronic cough is well known to hamper the psychological and social aspects of quality of life of a patient. Extensive research on chronic cough shows that the main neurobiological mechanism associated with chronic cough is loss of inhibitory control.
A group of researchers set out to understand if structural and functional changes related to chronic cough occur in higher cortical brain regions.
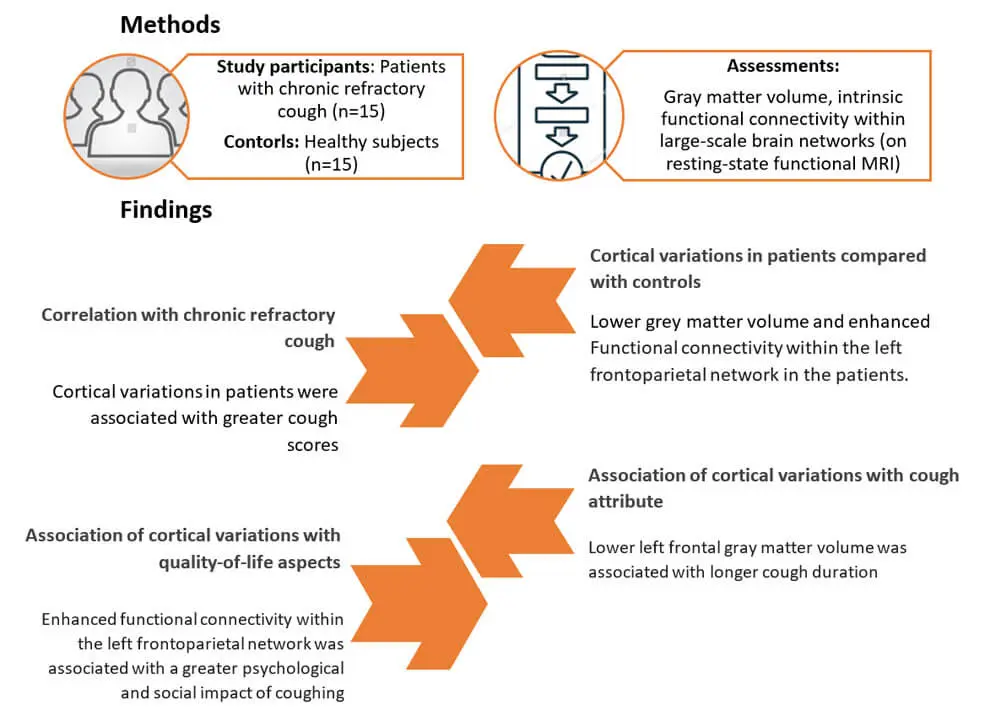
The findings of the above study open new avenues for research into strategies targeting the cognitive aspects of chronic coughing.
Reference: Namgung E, Song WJ, Kim YH, et al. Structural and functional correlates of higher cortical brain regions in chronic refractory cough. Chest. 2022;S0012–3692(22)00884–00894.
Effect of adenoidectomy on cough reflex sensitivity in children

Nasopharyngeal tonsil undergoes natural enlargement in children between the ages 3 to 5 years. When it is colonized by pathogenic bacteria, a series of physiological processes can lead to loss of immunity and the incidence of hypertrophy in the organ. Excessive hypertrophy of nasopharyngeal tonsil is termed adenoid hypertrophy (AH). Further, children are highly susceptible to chronic cough.
A group of researchers conducted a study to assess the effect of hypertrophied adenoid tissue in children on chronic cough reflex sensitivity.

The definition of the cough reflex sensitivity was the lowest capsaicin concentration that caused two (C2) or five (C5) coughs.
Results
- Cough reflex sensitivity increased (decrease in C2 and C5 values) after adenoidectomy in non-atopic children with chronic cough
– Cough reflex sensitivity for the C2 parameter was 31.86 (12.98–78.18) µmol/L preoperatively and 11.97 (6.16–23.26) µmol/L postoperatively (p=0.064)
– Cough reflex sensitivity for the C5 parameter was 234.91 (97.19–567.77) µmol/L preoperatively and 69.13 (29.08–164.35) µmol/L postoperatively (p=0.022) - After adenoidectomy, there was significant change in subjective cough assessment and a significant improvement in subjective AH symptoms
Adenoidectomy increased cough reflex sensitivity in this study. The results infer that presence of other frequent concomitant symptoms must be taken into consideration before indicating adenoidectomy.
Reference: Sojak J, Durdik P, Omar Mohamedova E, et al. Changes in cough reflex sensitivity in children after removal of hypertrophied adenoid tissue. J Asthma Allergy. 2022;15:517–524.
The patients’ perspective of chronic refractory cough

Understanding chronic refractory cough (CRC) from the patient’s viewpoint has several advantages:
- Aids health care providers to help the patient feel more supported
- Aids healthcare providers in recognizing the signs and symptoms sooner and appropriate referrals can be made sooner
There is limited information on the condition from the patient’s perspective.
A study was conducted to assess the features of CRC from the patients’ perspective.
Method

Study findings
- Onset of cough was reported by 19/20 participants; average total cough duration was 52 months.
- Inciting events of cough was reported by 14/20 participants; cold, upper respiratory infection (URI), pneumonia, and sinus infection were the most common inciting events.
- A total of 4 dominant themes, viz. cough triggers, physical symptoms, medical care, and quality of life were found.
Cough triggers
Vocalization, allergies, specific time of day or year, dryness, smells, exertion, and random triggers
Physical symptoms
Tickle in the throat, coughing fits, constant cough, dry cough, and uncontrollable cough exhaustion, voice changes, difficulty breathing
Medical care
Inhaler was the most common treatment; multiple treatment was prescribed in 87% patients; in 47% of the patients, cough frequency was reduced but not eliminated
Quality of life
55% of them described their coughs as “annoying,” whereas 35% of them reported frustration with their coughing. The most mentioned quality-of-life factors were social, including negative effect on social life (75%), criticizing comments from others (55%), feeling self-conscious about their cough (50%), sleep deprivation (40%), and everyday life interruptions (40%).
Understanding the patients’ perspective of chronic refractory cough can help the physicians understand the physical and emotional toll of the condition on the patients. Physicians can counsel patients appropriately to ease them of their apprehensions about their condition.
Reference: Wright ML, Fujiki RB, Lunga T, et al. Patient-reported qualitative analysis of chronic refractory cough. Am J Speech Lang Pathol. 2022:1–7.
Considering the multi-disciplinary approach in the management of chronic cough in children

Chronic cough (CC) is the most common reason for increased visits to pediatric and urgent care clinics.
Outcomes of CC include impaired quality of life, missed school days, inappropriate antibiotic usage, multiple physician visits in children.
The need for multi-disciplinary approach
A multi-disciplinary approach could be beneficial because:
- Conditions assessed and diagnosed by specialists could be different from those assessed by a general pediatrician
- Aids in early diagnosis and choosing appropriate treatment strategies
Otolaryngologists
- Aid in earlier identification of those cases of CC that require diagnostic work up and surgical intervention
Pulmonologists
- Important in cases of failure of the cough to resolve, recurrence, or concern for an underlying disease
- Diagnostic tests such as radiography (x-ray or CT), pulmonary function testing, and flexible bronchoscopy (FB) with broncho-alveolar lavage can be coordinated only with a pulmonologist
Gastroenterologists
- Important when GERD is the cause of CC
- GERD therapeutic approaches cannot be used for CC, until other clinical features of GERD are evident
- Detecting other features by esophagogastroduodenoscopy or endoscopy and further treatment requires a gastroenterologist
Studies evidence a 20%–40% cost savings for children who are managed comprehensively in a multidisciplinary setting compared to a single specialty evaluation. Several studies also support that a multi-disciplinary approach aids in correct diagnosis and adopting proper therapeutic strategies.
Appropriate referral and evaluation of persistent/recalcitrant cough by a multidisciplinary team may lead to earlier accurate diagnosis with likely cost savings.
Reference: Mukerji SS, Yenduri NJS, Chiou E, et al. A multi-disciplinary approach to chronic cough in children. Laryngoscope Investig Otolaryngol. 2022;7(2):409–416.
Assessment of the efficacy of pulmonary function test for accurate diagnosis of pediatric asthma and cough variant asthma

The symptoms of asthma and cough-variant asthma, common conditions in children, overlap those of other respiratory diseases. On the other hand, patients with COPD and asthma exhibit similar clinical symptoms. Compared to patients with COPD or asthma alone, patients
with asthma-COPD overlap have more frequent acute effects.
While pulmonary function tests are carried out to evaluate the clinical value of different types of respiratory diseases in children or infants, a group of researchers set out to clinically evaluate the efficacy of the pulmonary function tests.
Method
- For the pulmonary function tests, the researchers selected the COPD gene dataset and performed feature selection using the deep belief networks-support vector machines (DBN-SVM) scoring method.
- For analysis and comparison, they further built the differential diagnosis models using ROC curves.
- To assess the efficacy of the pulmonary function test, the researchers further conducted clinical diagnostic tests for pediatric asthma and cough variant asthma on two groups of children.
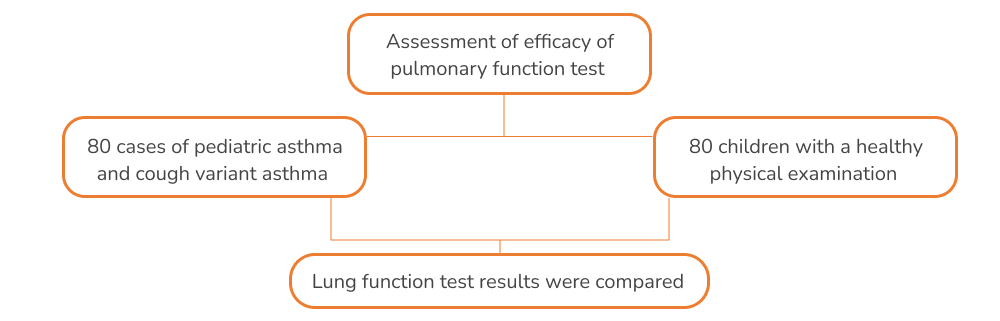
Result
The sensitive features associated with COPD and ACO classification using the deep belief network model were found to be in good agreement with known clinical diagnostic strategies.
Lung function rates between the groups
FEV1, PEF, and FVC levels were significantly lower (p<0.05), in healthy children. FEV1/FVC%, RV, and RV/TCL% were significantly higher (p<0.05) in children with asthma and cough variant asthma during acute exacerbation and chronic persistence.
Diagnostic rates of pulmonary function test vs. conventional test
The diagnostic rates of pulmonary function test for typical asthma and cough variant asthma were significantly higher than those of conventional tests (p<0.05).
Table 1. Comparison of the diagnostic accuracy of conventional examination and pulmonary function tests in children
- Routine inspection
- Pulmonary function test
- x²
- P value
Diagnostic rate
- 38()79.17
- 47()97.92
- -1.6318
- <0.05
Misdiagnosis rate
- 10(20.83)
- 1(2.08)
- 1.6318
- <0.05
Diagnostic rate
- 15(46.88)
- 30(93.75)
- -2.5154
- <0.05
Diagnostic rate
- 17(53.12)
- 2(6.25)
- 2.5158
- <0.05
Pulmonary function tests can accurately diagnose pediatric asthma and cough variant asthma. Further, the DBNs model could become a significant diagnostic decision aid.
Reference: Li H, Zhang X, Zhao Q, et al. Assessment of clinical diagnostic efficacy of pulmonary function test based on DBN-SVM of pediatric asthma and cough variant asthma. Comput Intell Neurosci. 2022;2022:1182114.
Pediatric chronic productive cough: Are antibiotics the solution?

Researchers have established that antibiotic therapy is effective in treating otherwise healthy young children with unexplained, prolonged wet cough of at least three weeks. The conclusion in an outcome of a meta-analytical study.
The meta-analysis
A group of researchers conducted a meta-analysis in 2018 using three randomized controlled trials to assess the efficacy of antibiotics in treating children with prolonged wet cough.
- Most children were 6 years old or younger.
- Wet cough lasted between 3 and 15 weeks.
- Amoxicillin/clavulanate 20 to 22.5 mg amoxicillin/kg twice daily were used for 7 to 14 days in two trials; erythromycin 50 mg/kg twice daily was used for 7 days in one trial.
- Analysis of data revealed results in favor of antibiotics as follows:
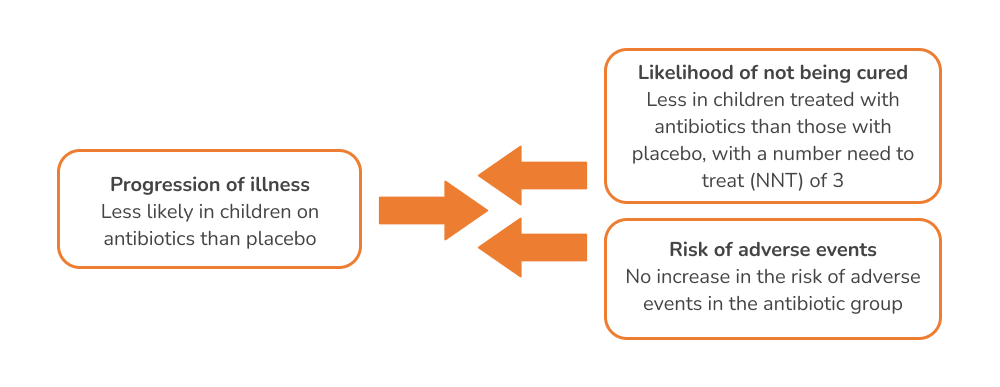
Other supporting results
Another group of researchers, in 2012, compared the efficacy of amoxicillin/clavulanic acid with placebo in 50 children with prolonged wet cough.
Children were randomized to receive amoxicillin/clavulanic acid 22.5 mg/kg twice daily for 14 days or placebo.
The primary outcome was cough resolution, defined as 75% improvement in the baseline cough score or cessation of coughing for at least three days, assessed at 14 days.
The study results are as follows:
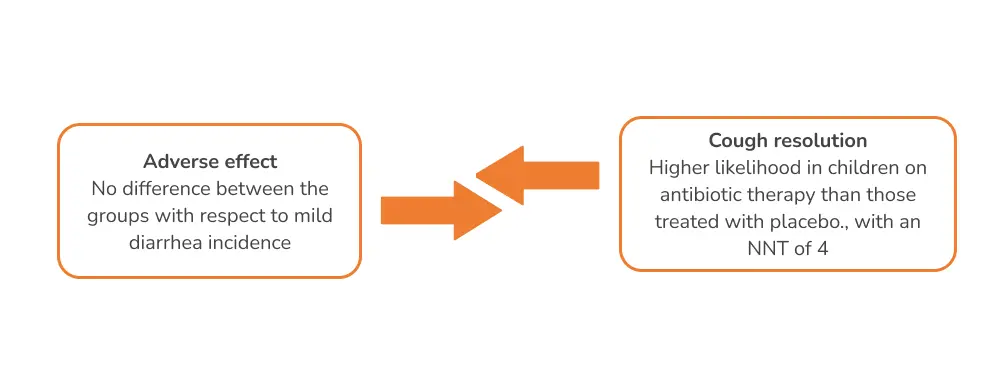
Antibiotics could be effective in achieving cough resolution and preventing the progression of illness.
Reference: Wipperman J, Ofei-Dodoo S, Nilsen K, et al. Are antibiotics effective in treating children with chronic productive cough? Evidence-Based Practice: 2022;25(4):32–33
Cough sensitivity: Evaluation methods and influencing factors

The most common way of objective cough assessment is the evaluation of cough sensitivity, the responsiveness of cough reflex to external stimuli. A higher cough sensitivity indicates that the cough receptors are sensitized, which results in responses to even weak stimuli that would not induce cough otherwise.
Evaluation methods of cough sensitivity
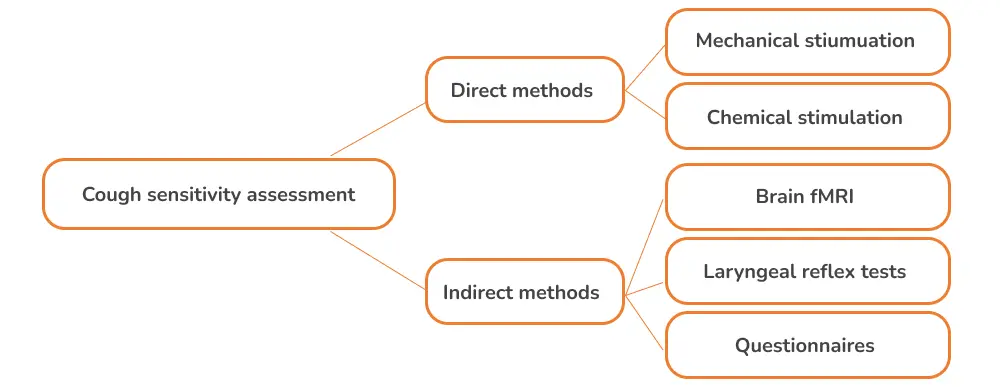
Mechanical stimulation
- Mechanical vibration is used to stimulate the cough receptors.
- The method is simple non-invasive, and safe.
- Some studies indicate that this method can distinguish healthy individuals from patients with cough hypersensitivity, to an extent. Further research is necessary to assess its investigative value.
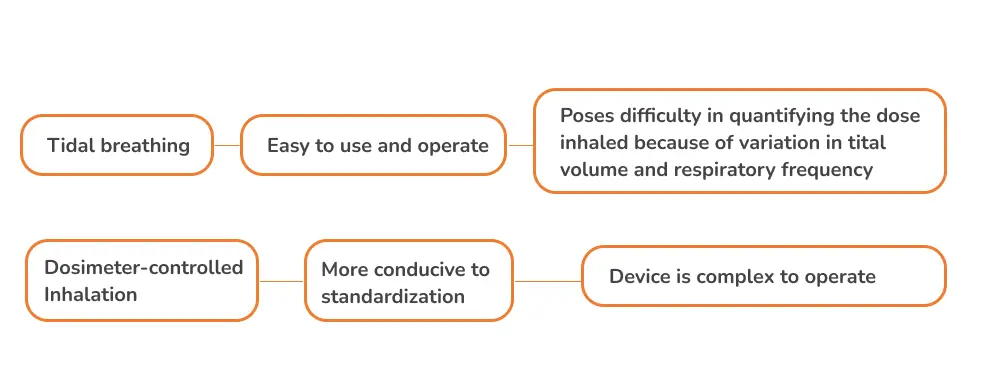
Chemical stimulation
- Widely used and proven.
- The subject inhales aerosol stimulant particles that further stimulates cough receptors and induces cough.
- Capsaicin is the most preferred chemical stimulant; it can be administrated via a tidal-breath inhalation or a dosimeter-controlled inhalation.
- Factors such as, smoking, obesity, sex, allergic inflammation, TRPV1 polymorphisms, and chemosensory regulation affect cough sensitivity assessment.
Brain fMRI
- A specific sensory organ is stimulated to cause neural activity in the corresponding cerebral cortex, which is detected on fMRI. Thus, fMRI helps in the indirect assessment of cough sensitivity.
- Aids in assessing cough hypersensitivity at the central level and further development of novel antitussives.
Laryngeal reflex tests
- Laryngeal hypersensitivity is an excessive laryngeal response to external stimuli.
- It is an indirect indicator of cough hypersensitivity; this is indicated by resolution of laryngeal irritation after treatment of cough.
- Researchers have developed a novel laryngopharyngeal endoscopic esthesiometer and rangefinder (LPEER); however, the device has been evaluated in patients with swallowing difficulties and not in patients with chronic cough.
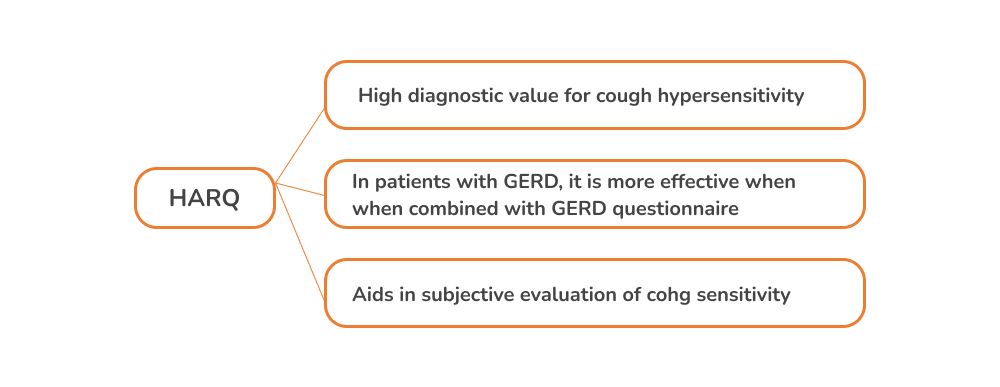
Questionnaires
- These reflect cough sensitivity from different perspectives.
- Hull airway reflux questionnaire (HARQ) was developed to evaluate cough sensitivity and diagnose CHS.
Several cough sensitivity assessment methods exist; however, each method must be thoroughly researched with more studies to assess appropriate applicability.
Reference: Mei H, Gu W, Ran L, et al. Evaluation methods and influencing factors of cough sensitivity. Ther Adv Respir Dis. 2022;16:17534666211070134.

An initiative by Glenmark to educate about everything related to Cough and spread awareness about cough related health conditions.
Quick Links
Contacts
- GLENMARK PHARMACEUTICALS LIMITED Glenmark Corporate Enclave, BD Sawant Marg, Chakala, Off WE Highway, Andheri (E), Mumbai 400099
- Terms & Condition
- Privacy Policy
- Sitemap
- Disclaimer
- Coughology © 2024 All Right Reserved
