Conference Updates
- Cough frequency in COPD with frequent sputum production
- Cough acoustics in patients with COVID-19
- Blood eosinophil count and response to oral corticosteroids in children admitted with acute preschool wheeze
- Efficacy of omalizumab in asthma control
- Ventilation and perfusion abnormalities in the post-recovery phase of noncritical COVID-19
Cough frequency in COPD with frequent sputum production
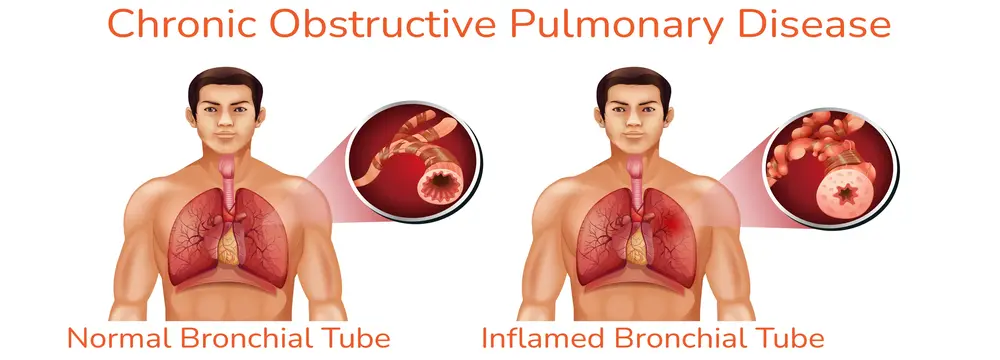
Not much is known about cough frequency and characteristics in patients with chronic obstructive pulmonary disease (COPD) and the effect of cough events on sleep efficiency.
Study
- A group of researchers assessed the relationship between nocturnal cough frequency and sleep disturbance in patients with COPD and regular sputum production.
- The study was a sub-study of the baseline population from the O-COPD trial, which recruited 45 stable patients with COPD with a productive cough.
- The participants were stratified according to the self-sputum scale into daily sputum producers (DSP) or not daily sputum producers (NDSP).
Study findings
- The frequency of cough was higher during day than at night in the DSP group
- Increased frequencies of getting out of the bed and body transitions in the DSP group
- Cough frequency at night was significantly associated with getting out of the bed, sitting transitions, and total body transitions
Subjective and objective cough monitoring in patients with COPD offers a better understanding of cough severity and frequency, and associated disturbances such as sleep disturbance and frequent body movements at night.
Reference: Alghamdi SM, Philip KE, Alsulayyim AS, et al. Presented at American Thoracic Society International Conference, May 13-18, 2022
Cough acoustics in patients with COVID-19

While cough is a predominant symptom in COVID-19 patients, assessing acoustics could potentially offer information about the events occurring in the respiratory system during COVID-19.
Study
A group of researchers analyzed the acoustic findings of cough signals in patients hospitalized due to COVID-19.
A built-in microphone of a simple smartphone was used to record coughs. Recording was done in 2 groups of patients representing 2 different stages of COVID-19.

Cough sounds were recorded at 48 kHz and segmented into 3 parts: the first cough sound, the intermediate part, and the second cough sound.
Study findings
This indicates that cough acoustic characteristics vary at different stages of the disease in patients with COVID-19.
Recording and assessing cough characteristics is a novel way of understanding respiratory mechanics in patients with COVID-19.
Reference: Caguana Vélez OA, Davidson C, Lozano M, et al. Presented at American Thoracic Society International Conference, May 13–18, 2022.
Blood eosinophil count and response to oral corticosteroids in children admitted with acute preschool wheeze

Even though oral corticosteroid usage is ineffective in treating acute wheeze attacks, children in hospitals are often treated with oral corticosteroids.
Study
A group of researchers conducted a study to assess if children with peripheral eosinophilia admitted with acute wheeze show a differential response to treatment with oral corticosteroids as indicated by length of stay.
Length of stay was calculated as the time between treatment initiation and decision to discharge.
Study findings
- A total of 82 children had an eosinophil count recorded and received oral corticosteroid treatment.
- 26.8% (22/82) belonged to the eosinophil-high group and 73.1% (60/82) to the eosinophil-low group.
- There was no significant difference in the median length of stay between two groups (median stay 41.5 hours vs. 46.75 hours).
There was no significant difference in the length of stay of preschool children admitted with acute wheeze and treated with oral corticosteroids as determined by blood eosinophil count. Identifying larger cohorts, and comparisons of length of stay including children not treated with oral corticosteroids in both eosinophil high and eosinophil low groups may be helpful.
Reference: Manzoor J, Gupta A, Cook J. Presented at the 8th King’s John Price Paediatric Respiratory Conference (KJPPR); London, United Kingdom; June 16–17, 2022.
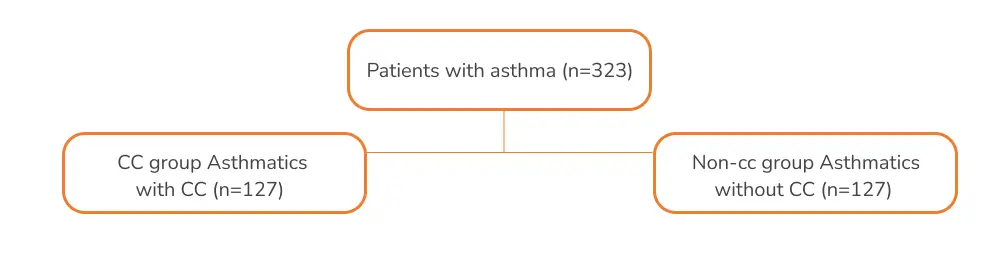
Efficacy of omalizumab in asthma control

The long-term efficacy of omalizumab in children and adolescents with asthma in real life settings is unknown.
Study
- A study was conducted to assess if omalizumab can offer long-term and sustained efficacy by means of maintaining good asthma control.
- The study was a multi-centre case note review of children (aged <18 years; n=79), who were on omalizumab for persistent allergic asthma.
- The mean IgE at baseline was 1000 (57-1300).
- The total mean daily inhaled corticosteroids (ICS) dose equivalent to fluticasone propionate was 617mcg (400-1000); 37 patients (47%) were receiving daily oral steroids at baseline.
Study findings
Change in the number of patients receiving oral steoids
- NUmber of patients reduced from 17 at 1 year to 9 at 24 months.
Courses of oral corticosteroids (OCS) for exacerbations
- Reduced from median of 6 during a period of 12 months before omalizumab to 1 during the first 12 months after omalizumab
Mean astham control test (ACT)
- Scores increased from 12 to 18 (baseline vs. at 12 months)
Proportion of “well controlled” patients
- 46% of patients receiving omalizumab at 12 months could meet the definition of “well controlled
Omalizumab was able to improve asthma control in ~50% of the patients and most of them on OCS were able to stop over time. In several patients, there was a suboptimal control.
Reference: Gregson EC, Tang A, Brookman S, et al.
Presented at the 8th King’s John Price Paediatric Respiratory Conference (KJPPR); London, United Kingdom; June 16–17, 2022.
Ventilation and perfusion abnormalities in the post-recovery phase of noncritical COVID-19

A small lung functional imaging study shows that ventilation is impaired in patients with no history of lung disease recovering from noncritical COVID-19.
Study
A study was conducted to assess the prevalence and clinical relevance of ventilation (V) and perfusion (Q) impairment in individuals with no history of lung disease 4-weeks after recovery from noncritical COVID-19.
Study findings
Hospitalization and isolation
- that 9/25 post-COVID-19 patients were hospitalized and 16/25 of them were home isolated during acute infection
Ventilation defects
- 88% of the hospitalized vs. 44% of home-isolated participants of the post-COVID-19 groups vs. 30% in controls
Ventilatio- associated heterogeneity
- Greater in hospitalized (P = 0.003), but not home-isolated participants, compared to the never-COVID-19 controls
A correlation was established between post-COVID-19 ventilation-heterogeneity and the dyspnea-scale, SGRQ-score, 6MWD, SpO2, CT parenchymal opacities, and neutrophil percentage.
The study provides evidence for the presence of ventilation impairment in post-COVID-19 patients that had a positive relationship with parenchymal opacities, respiratory symptoms and exercise-capacity.
Reference: Venegas C, Marriott CJ, Ho T, et al. Presented in the Canadian Respiratory Conference, April 7-9, 2022.
An initiative by Glenmark to educate about everything related to Cough and spread awareness about cough related health conditions.
Quick Links
Contacts
- GLENMARK PHARMACEUTICALS LIMITED Glenmark Corporate Enclave, BD Sawant Marg, Chakala, Off WE Highway, Andheri (E), Mumbai 400099
- Terms & Condition
- Privacy Policy
- Sitemap
- Disclaimer
- Coughology © 2024 All Right Reserved
